Why we need to prioritise support after the pandemic
15 October 2021

By Associate Professor Muhammad Aziz Rahman
The ongoing COVID-19 pandemic is occurring in waves and impacting the psychological well-being of global populations. Varying degrees of restrictions and lockdowns, social isolation, financial loss and disruption of daily routine for prolonged periods — and the fear of contracting the virus — are the primary reasons for COVID-related stress.
While the evidence on factors associated with psychological well-being because of the COVID-19 pandemic was limited at the beginning of the pandemic, a team of researchers from the School of Health investigated the issue in Australia during 2020. The team found that people with higher psychological distress increased smoking and alcohol consumption during the pandemic period. Females and people with pre-existing mental health conditions were more likely to experience higher levels of psychological distress. The study was published in the BMC Globalization and Health journal in October 2020.
These findings led the team to examine the issue globally. Most published studies have examined the psychological impacts of COVID-19 in a single country or small communities, and evidence from multicultural communities on a worldwide scale has been lacking. It is essential to generate this evidence for the early identification of vulnerable groups and to help them avoid these long-term impacts in the post-pandemic period.
A study was planned with existing and new research collaborators globally to examine the extent of, and the factors associated with psychological distress, the level of fear of COVID-19 and coping strategies among a diverse range of people in multi-country settings. BMC Globalization and Health published the study in October 2021, one of the few large-scale global studies published so far.
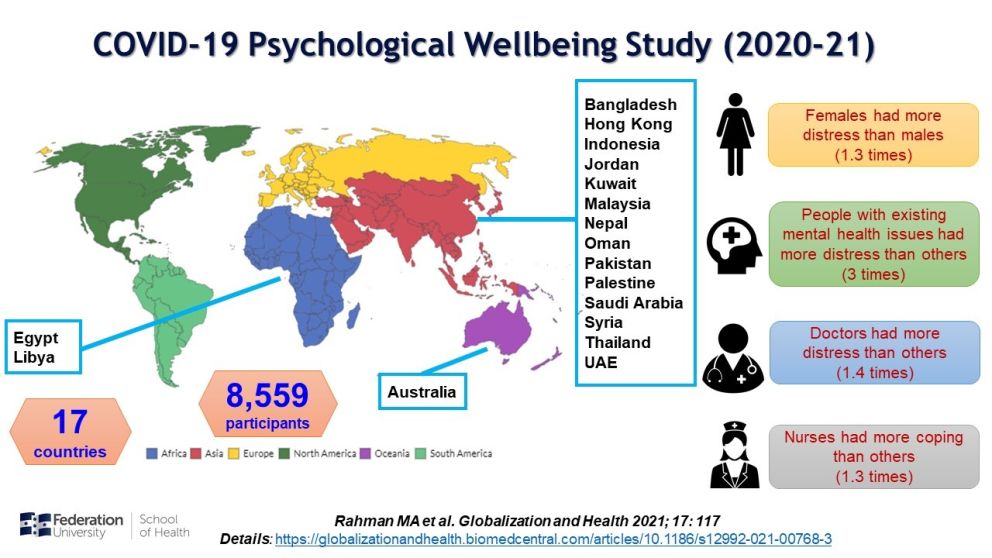
A web-based survey was conducted with study participants from Australia, Bangladesh, Egypt, China (Hong Kong), Indonesia, Jordan, Kuwait, Libya, Malaysia, Nepal, Oman, Pakistan, Palestine, Saudi Arabia, Syria, Thailand, and the United Arab Emirates (UAE). Any adult aged 18 or above was eligible to participate in the anonymous survey.
Among the 8,559 study participants, more than two-thirds experienced moderate-to-very-high levels of psychological distress, a quarter had high levels of fear of COVID-19, and more than half of the study population exhibited a greater ability to cope during the pandemic.
The lowest prevalence of moderate-to-very-high levels of distress was reported from Thailand and the highest from Egypt; the lowest level of fear was reported from Libya and the highest from Bangladesh; the lowest coping was reported from Australia and the highest from Syria.
When we controlled all the sociodemographic variables, few findings were similar to the Australian study. Females, people with pre-existing mental health conditions and those who perceived distress due to change of employment, had higher levels of both distress and fear of COVID-19. Doctors had higher levels of psychological distress but low levels of fear of COVID-19. On the other hand, nurses had medium to high resilient coping.
 Women are disproportionately affected with psychological distress during the current COVID-19 pandemic in Australia and globally. Studies from other countries also confirmed female gender was a consistent predictor for psychological distress.
Women are disproportionately affected with psychological distress during the current COVID-19 pandemic in Australia and globally. Studies from other countries also confirmed female gender was a consistent predictor for psychological distress.
Apart from the stressor factors common in both genders, the primary caregiver roles in a household and delayed healthcare-seeking behaviour could contribute to the higher psychological distress among women. It warrants particular attention for planning gender-specific support strategies across all the countries during the post-pandemic period.
People with pre-existing mental health conditions had to face the double burden of disease due to the additional distress associated with the pandemic. Social distancing, the lack of face-to-face interactions, challenging accessibility to healthcare providers, and non-preference of teleconsultations could have impacted their medications adherence and worsened their existing conditions. The issue of social stigma, specifically within multicultural communities in Australia, cannot be ignored as well. This requires support from the community leaders and improved awareness on existing resources including Head to Health.
Within the ongoing pandemic, this unfunded study across 17 countries within a short period was made possible by the in-kind support of researchers and international collaborators. The findings of this study indicate an urgent need to prioritise those vulnerable populations. Adequate medical and social support and specific health promotion policies should be considered within the strategic response to the ongoing pandemic and future crises.
Dr Muhammad Aziz Rahman is an Associate Professor of Public Health and Associate Dean Research at School of Health. Researchers who contributed to the study include: Professor Wendy Cross, Adjunct Associate Professor Mimmie Watts, Dr Louisa Lam, Dr Biswajit Banik, Dr Bindu Joseph and Dr Masudus Salehin.
Related reading:
Smoking and alcohol consumption increases amid COVID-related distress
Let’s stop self-isolating when we no longer have to self-isolate


